Mikroszkópos gyökérkezelés
Mikroszkópos gyökérkezeléssel több fogat menthetünk meg. Legyen szó újrakezelésről, vagy első gyökérkezelésről, ez a legjobb gyökérkezelési módszer!
Mikroszkópos
Gyökérkezelés előnyei és menete
Egy fog, amit elsőre mikroszkópos technikával kezelnek, 90% felett sikeres lesz!
Speciális orvosi tudás
Ön egy specialista szaktudását kapja, tehát az orvos, aki kezelni fogja, többet tud a gyökérkezelés szakterületéről mint más, nem erre a területre specializált fogorvos.
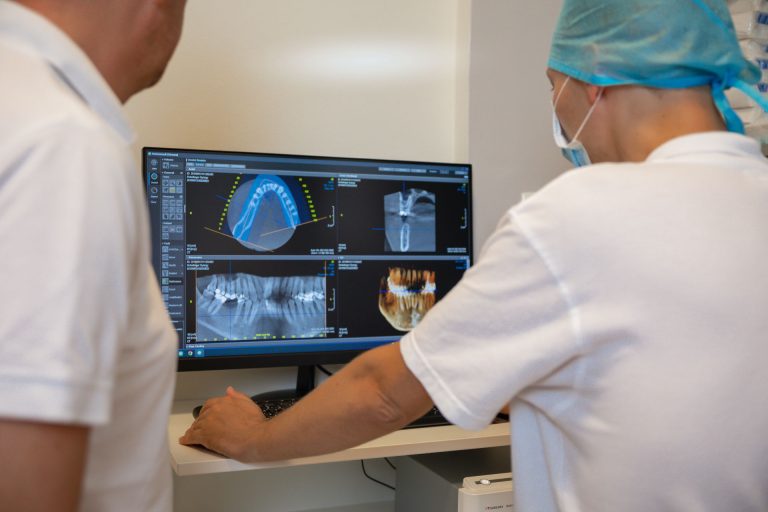
20-szoros nagyítás
A kezelendő fogát orvosa akár 20-szoros nagyításban kezeli. A gyökércsatornák milliméteres világában bizonyára Ön is el tudja képzelni mit jelent ez a szabad szemmel történő, hagyományos gyökérkezelés “tapogatózásához” képest.
Hatékony fertőtlenítés
A mikroszkópos gyökérkezelés biztonságosabb és hatékonyabb fertőtlenítési protokollt tartalmaz, mint a hagyományos kezelés. Ez a 3D ultrahangos fertőtlenítés, mely a teljes csatornarendszert átjáró fertőtlenítéshez nagyban hozzájárul!
A kezelés menete
A mikroszkópos gyökérkezelés általában 2-4 alkalom. Egy ülés általában 90 perces. A folyamat során a gyökércsatornák feltárása, speciális, 3D ultrahangos fertőtlenítése történik és biokerámia gyökértöméssel zárul.
Gyökérkezelés utáni teendők
A gyökérkezelés után további kezelés szükséges a koronai rész helyreállítására. Ez történhet biomimetikus fogtöméssel, koronával, vagy betéttel, mely már egy másik fogorvos szakterületéhez tartozik.

Árak
Mikroszkópos gyökérkezelés
A mikroszkópos gyökérkezelés speciális eszközigénye, illetve a hosszabb kezelési időtartam miatt a hagyományos kezelésnél drágább. Pontos árakat az állapotfelmérés után a kezelési terv tartalmaz.
Mikroszkópos gyökérkezelés – kezelésfolyamat indítása – első ülés
A legnagyobb sikerességet nyújtó, mikroszkópos gyökérkezelés. A kezelésre vonatkozó fogászati árak az alábbiakat tartalmazzák: Nagy nagyítású operációs mikroszkóppal végzett gyökérkezelés első, bevezető ülése,. Kofferdam izolálásban. speciális titán műszerekkel történő feltárás, 3D ultrahangos fertőtlenítés és gyógyszeres lezárás. Az ár a gyökércsatornák számától függően változik.
Bővebben62.000 Ft - 95.000 Ft
Mikroszkópos gyökértömés – kezelésfolyamat lezárása
Biokerámia gyökértöméssel. A kezelésre vonatkozó fogászati árak az alábbiakat tartalmazzák: 3D ultrahangos fertőtlenítés, biokerámia gyökértömés. Az ár a gyökércsatornák számától függ. A végleges restauráció további kezelést igényel, pl. fogtömés, onlay vagy korona, melyek árát a kezelés nem tartalmazza.
Bővebben62.000 Ft - 95.000 Ft

Új páciensek részére
Először jár nálunk?
Nézze meg új pácienseink részére ajánlott aktuális csomagjainkat.
Jelentkezzen állapotfelmérésre!
Egyeztesse munkatársainkkal a fogazatával kapcsolatos elképzelését, akik orvoscsapatunk legmegfelelőbb tagját ajánlják majd az állapotfelmérés elvégzésére. Ezután az adott szakmai területen leginkább jártas fogorvosunk végzi el a kezelését.
Rendelőnk
1137 Budapest
Szent István körút 10. 3.em 8.
Nyitvatartás
H – Cs: 08:00 – 20:00
P: 09:00 – 15:00
Szo – V: Zárva
Orvosaink
Fogorvos csapatunk
Referenciák
Fedezze fel Ön is a cirkónium korona vagy az üvegkerámia héj lehetőségeit. Nézze meg esetbemutatásainkat!
Rólunk mondták
Nagyon nem szívesen járok fogorvoshoz és sajnos amúgy is tű fóbiás vagyok, nem jó kombináció! Nevelőapám és Öcsém ajánlották a Bp. Dentalt, és szerintem még életemben nem jöttem ki mosolyogva egy fogorvosi rendelőből. A Doktornő nagyon profi, mindent elmagyaráz, percek alatt kész voltunk. Az Asszisztens Hölgy is rendkívül segítőkész volt! Amúgy is, mintha egy nyugati országban jártam volna, mindenki udvarias, mosolyog, a szolgáltatás pedig magas színvonalú. Csak ajánlani tudom mindenkinek.
Mindenkinek ajánlom a Budapest Dental fogászatot, kedves, türelmes, profi orvosok, személyzet, külön köszönöm Dr. Némethy Miklósnak, hogy minden kezelési lehetőséget részletesen elmagyaráz.
Maximálisan elégedett vagyok az itt kapott kezelésekkel és hálásan köszönöm Dr. Némethy Miklósnak a kiváló munkáját, türelmét és precizitását. Továbbá köszönöm kedvességet és rugalmasságot amit minden egyes időpontfoglalás során megtapasztalok.
Amióta ide járok már nincs gyomorgörcsöm mikor elindulok a kezelésre. Itt figyelnek az igényeimre és annyira kíméletesen végzik a munkát amennyire csak lehet.
Nagyon elégedett voltam. Mindenki mindig nagyon kedves volt, soha nem kellett sokat várni, soha nem fájt semmi és egyszer sem mentem oda úgy, hogy „jaj, már megint fogászatra kell mennem”. ?
Hosszú ideje a legjobb szolgáltatást nyújtják. A rendelők kiválóan felszereltek, ami a modern fogászathoz szükséges, azzal rendelkeznek. A kezelés fájdalommentes, a személyzet kedves, és türelmes.
Kikhez volt szerencsém?
Időrendben: recepciósok, Dr. Déry Judit és asszisztense, Dr. Schreindorfer Károly és asszisztense. Nem tudom, hogy mit emeljek ki: a szakértelmet, a kedvességet vagy a mentalitást.
Megnyugtató, kellemes, tiszta környezet, a személyzet, az orvosok nagyon kedvesek, segítőkészek. Érezni lehet a szakértelmet, a törődést. A problémámat fájdalommentesen, elsőre megoldották. Köszönöm a munkájukat!
Nagyon hálás vagyok azért, hogy teljesen véletlenül rátaláltam a fogászatra, és már pár alkalom után aggodalom nélkül jártam a kezelésekre (ami konkrétan korábban nálam a pánik félelmet jelentette az addigi tapasztalatok után más fogászatokon). Ha már sok-sok évvel ezelőtt ilyen remek kezekbe kerültem volna, sokkal kevesebb problémám alakult volna ki. […]

Speciális tudás
Nálunk nincs futószalag, a minőségi fogászathoz idő kell
A mikroszkópos gyökérkezelés kivitelezése speciális szakértelmet igényel. Rendszerint azok a fogorvosok mélyülnek el ezen a szakterületen, akik biztonságosabbat, sikeresebbet akarnak annál, mint amire a hagyományos fogászat képes. Az ilyen munka több időt, nagyobb precizitást kér a fogorvostól és nagyobb türelmet a pácienstől.
Rendelőnk kifejezetten specializálódott a kritikus állapotú fogak megmentésére. Ha szeretne többet megtudni a mikroszkópos fogászati kezelésekről, olvassa el blogcikkünket!
Tudjon meg többet problémájáról
Szeretne megbízható helyről tájékozódni fogászati kihívását illetően? Közérthető szakmai írásainkból minden kiderül. A cikkeket tapasztalt fogorvosok írják!