Fogtömés,
gyökérkezelés
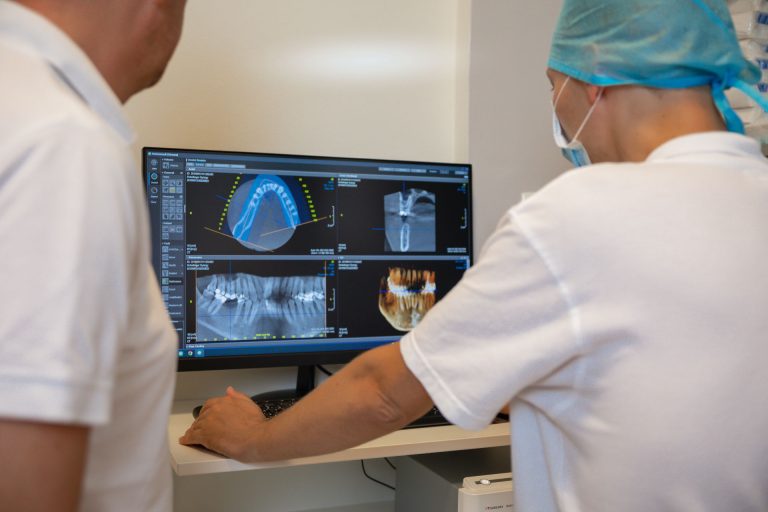
A fogászat lényege az egészséges mosoly életre szóló megtartása! Rendelőnk specializálódott a valóban hatékony fogmegtartó kezelésekre és a kritikus állapotú fogak megmentésére.
Mely kezeléseink közül választhat?
Fogtömés fájdalom nélkül
Ha már szuvas a fog, kérjen minőségi, tartós fogtömést, tartsa meg fogait és csökkentse a hosszú távú fogászati költségeit!
Miért ezt válassza?

Új páciensek részére
Először jár nálunk?
Nézze meg új pácienseink részére ajánlott aktuális csomagjainkat.
Jelentkezzen állapotfelmérésre!
Egyeztesse munkatársainkkal a fogazatával kapcsolatos elképzelését, akik orvoscsapatunk legmegfelelőbb tagját ajánlják majd az állapotfelmérés elvégzésére. Ezután az adott szakmai területen leginkább jártas fogorvosunk végzi el a kezelését.
Rendelőnk
1137 Budapest
Szent István körút 10. 3.em 8.
Nyitvatartás
H – Cs: 08:00 – 20:00
P: 09:00 – 15:00
Szo – V: Zárva
Orvosaink
Fogorvos csapatunk
Referenciák
Fedezze fel Ön is a cirkónium korona vagy az üvegkerámia héj lehetőségeit. Nézze meg esetbemutatásainkat!
Rólunk mondták
Nagyon nem szívesen járok fogorvoshoz és sajnos amúgy is tű fóbiás vagyok, nem jó kombináció! Nevelőapám és Öcsém ajánlották a Bp. Dentalt, és szerintem még életemben nem jöttem ki mosolyogva egy fogorvosi rendelőből. A Doktornő nagyon profi, mindent elmagyaráz, percek alatt kész voltunk. Az Asszisztens Hölgy is rendkívül segítőkész volt! Amúgy is, mintha egy nyugati országban jártam volna, mindenki udvarias, mosolyog, a szolgáltatás pedig magas színvonalú. Csak ajánlani tudom mindenkinek.
Mindenkinek ajánlom a Budapest Dental fogászatot, kedves, türelmes, profi orvosok, személyzet, külön köszönöm Dr. Némethy Miklósnak, hogy minden kezelési lehetőséget részletesen elmagyaráz.
Maximálisan elégedett vagyok az itt kapott kezelésekkel és hálásan köszönöm Dr. Némethy Miklósnak a kiváló munkáját, türelmét és precizitását. Továbbá köszönöm kedvességet és rugalmasságot amit minden egyes időpontfoglalás során megtapasztalok.
Amióta ide járok már nincs gyomorgörcsöm mikor elindulok a kezelésre. Itt figyelnek az igényeimre és annyira kíméletesen végzik a munkát amennyire csak lehet.
Nagyon elégedett voltam. Mindenki mindig nagyon kedves volt, soha nem kellett sokat várni, soha nem fájt semmi és egyszer sem mentem oda úgy, hogy „jaj, már megint fogászatra kell mennem”. ?
Hosszú ideje a legjobb szolgáltatást nyújtják. A rendelők kiválóan felszereltek, ami a modern fogászathoz szükséges, azzal rendelkeznek. A kezelés fájdalommentes, a személyzet kedves, és türelmes.
Kikhez volt szerencsém?
Időrendben: recepciósok, Dr. Déry Judit és asszisztense, Dr. Schreindorfer Károly és asszisztense. Nem tudom, hogy mit emeljek ki: a szakértelmet, a kedvességet vagy a mentalitást.
Megnyugtató, kellemes, tiszta környezet, a személyzet, az orvosok nagyon kedvesek, segítőkészek. Érezni lehet a szakértelmet, a törődést. A problémámat fájdalommentesen, elsőre megoldották. Köszönöm a munkájukat!
Nagyon hálás vagyok azért, hogy teljesen véletlenül rátaláltam a fogászatra, és már pár alkalom után aggodalom nélkül jártam a kezelésekre (ami konkrétan korábban nálam a pánik félelmet jelentette az addigi tapasztalatok után más fogászatokon). Ha már sok-sok évvel ezelőtt ilyen remek kezekbe kerültem volna, sokkal kevesebb problémám alakult volna ki. […]
Tudjon meg többet problémájáról
Szeretne megbízható helyről tájékozódni fogászati kihívását illetően? Közérthető szakmai írásainkból minden kiderül. A cikkeket tapasztalt fogorvosok írják!